Connect With Us
Featured Articles

Common Causes of Swollen Feet

Swollen feet can be caused by several factors, often linked to underlying health conditions. One common cause is leaky veins, where blood flows backward due to weakened valves, leading to fluid buildup in the lower limbs. This condition, known as venous insufficiency, is often accompanied by discomfort and swelling. Another factor to consider is the side effects of medication. Certain drugs, such as those used for high blood pressure or diabetes, can cause fluid retention, leading to swelling in the feet. Dependent edema is another possible cause, particularly for individuals who spend prolonged periods standing or sitting. This condition results from gravity pulling fluid into the lower extremities. Lastly, inflammation due to injury, infection, or conditions like arthritis can cause swelling in the feet. If you have swollen feet, it is suggested that you consult a podiatrist who can determine what the reason is, and offer effective relief and treatment tips.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact one of our podiatrists of New England Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
- Phlebitis - A condition that causes the veins to become inflamed and can also cause leg pain.
- Liver disease - This may lead to low blood levels of albumin which is a protein. This can cause fluid in the blood to pass into the tissues and several areas of the body can become swollen.
- Heart failure - When the heart doesn’t pump properly the blood that is normally pumped back to the heart can pool in the veins of the legs causing swollen feet.
- Kidney disease - One of the main functions of the kidneys is releasing excess fluid in the body. This type of condition can make it difficult for the kidneys to function properly, and as a result the feet may become swollen.
- Deep-vein thrombosis (DVT)- This is a serious condition where blood clots form in the veins of the legs. They can block the return of blood from the legs to the heart which may cause the feet to swell. It is important to be treated by a podiatrist if this condition is present.
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please feel free to contact one of our offices located in Chelmsford and Newburyport, MA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Swelling of the Feet
There are many reasons why patients experience swelling of the feet. It is rather common and may be a side effect of pregnancy or from sitting and standing for most of the day. Gravity could also play a role in the development of swollen feet. It is known that the weight of blood volume in our bodies is exerted on the veins in the legs and feet. The veins may not work as efficiently during the aging process, and this could make the blood flow backward causing swollen feet. Relief may be found when obese patients lose weight, and it may help to engage in compression therapy by wearing compression socks, stockings, or athletic sleeves. This method can release pressure on the feet and ankles which may help to reduce existing swelling. There are patients who have controlled their swollen feet by implementing healthy lifestyle changes. These can consist of reducing salt intake, incorporating a gentle exercise regime into the daily routine, and drinking plenty of fresh water. Swollen feet may be a temporary condition that affects people who travel via airplane or automobile, so it is beneficial to walk as frequently as possible even though it can be difficult. Swelling of the feet can also be indicative of other health issues so it is important to pay attention to any type of chest pain, mental confusion, dizziness, or fever. If you consistently have swollen feet, it is strongly suggested that you consult with a podiatrist who can help determine the cause and how to effectively treat it.
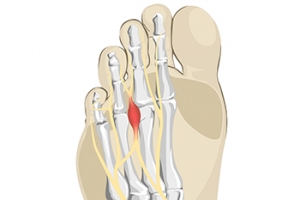
Causes and Signs of Morton’s Neuroma
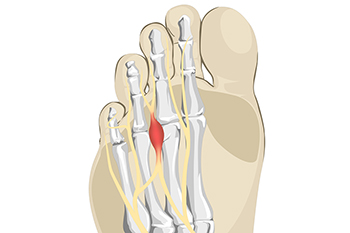
Morton's neuroma is a condition that affects the foot, causing pain and discomfort due to a thickening of the tissue surrounding one of the nerves leading to the toes. This condition typically occurs between the third and fourth toes, and is often described as feeling like there is a small stone or bump in the shoe. The exact cause of Morton's neuroma is not always clear, but it is often linked to repetitive stress or irritation to the nerves in the foot. High heels, tight shoes, and activities that put pressure on the toes, such as running or jumping, can increase the risk. Common signs of Morton's neuroma include sharp, burning pain in the ball of the foot and tingling, or numbness in the toes. The pain may worsen when walking or standing for extended periods. If you have pain in this part of your foot, it is suggested that you consult a podiatrist who can accurately diagnose and treat what may be going on.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of New England Foot and Ankle. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact one of our offices located in Chelmsford and Newburyport, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
What Is Plantar Fasciitis?

Plantar fasciitis is a foot condition that causes pain in the heel and along the bottom of the foot. It occurs when the plantar fascia, a thick band of tissue that connects the heel bone to the toes, becomes inflamed. The primary symptom of plantar fasciitis is sharp heel pain, especially when taking the first steps in the morning or after prolonged sitting. The pain may decrease after walking but can return after long periods of standing or physical activity. Common causes of plantar fasciitis include overuse, poor footwear, tight calf muscles, and abnormal foot mechanics, such as flat feet or high arches. Additionally, obesity, aging, and activities that place excessive pressure on the feet, like running or standing for long hours, can increase the risk of developing this painful condition. Plantar fasciitis can cause pain and discomfort, and it may be difficult to complete daily activities. If you have heel pain, it is suggested that you consult a podiatrist who can provide an accurate diagnosis and treatment.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from New England Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact one of our offices located in Chelmsford and Newburyport, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Onychomycosis and the Effectiveness of Laser Treatment

Onychomycosis is a fungal infection that causes the nails to become discolored, thickened, and brittle. This condition is commonly found in toenails but can also affect fingernails. The infection occurs when fungi, typically dermatophytes, invade the nail bed leading to visible damage. Traditional treatments for onychomycosis include antifungal creams and oral medications, but they may take time or have side effects. Laser treatment has become an effective alternative, as it uses targeted light to penetrate the nail and destroy the fungus without harming surrounding tissue. The heat from the laser kills the fungal cells, promoting healing and reducing the risk of recurrence. Laser treatment for onychomycosis is generally safe, with minimal side effects, and can offer quicker results than n other treatments, making it a popular choice for those seeking relief from this persistent condition. If you have developed toenail fungus, it is suggested that you contact a podiatrist who can discuss whether laser treatment is right for you.
Laser treatment can be an effective way to get rid of toenail fungus. If you have any questions about laser treatment, consult with one of our podiatrists from New England Foot and Ankle. Our doctors will assess your condition and provide you with quality treatment for fungal nails.
What Are Toenail Fungal Infections?
Onychomycosis, or fungal infection of the nail, is a relatively common and non-serious condition. Around 10 percent of U.S. citizens are afflicted with fungal nails. Common forms of fungus that infect the nail include dermatophytes, yeasts, and molds.
Symptoms of Toenail Fungal Infections Include:
- Nail thickening
- Brittleness of the nail
- Discoloration of the nail
Diagnosis for Fungal Nails
Fungal infections are diagnosed by fungal culture and microscopy. This will rule out any other conditions such as nail trauma, psoriasis, lichen planus, and onychogryphosis.
What Is Laser Treatment?
Laser treatment is a non-invasive, safe, quick, and painless procedure that uses the heat from a laser to kill fungus in the nail. Each infected nail is targeted with a laser for several minutes. The treatment is usually utilized several different times over a select period. During this time, a podiatrist will keep an eye on the infection.
If you have any questions, please feel free to contact one of our offices located in Chelmsford and Newburyport, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Laser Treatment for Fungal Nails
A new treatment for fungal nails, or onychomycosis, which has grown in popularity in recent years, is laser treatment. Laser treatment involves the use of a laser that kills fungus in the toenail with heat. Laser therapy causes no side effects and does not affect nearby healthy tissue.
Toenail fungus afflicts almost 10 percent of the U.S. population and is more common among the elderly. The most common symptom of toenail fungus is the discoloration and thickening of the nail. The nail can also become brittle and a foul smell may be produced. In rare cases, pain might be present. While it is not a serious condition, it can lead to a perception of disgust amongst those it affects. There are several different fungi that cause fungal infections. These include dermatophyte, yeast, and mold. The most common of these is dermatophyte.
Diagnosis for fungal nails involves a podiatrist utilizing microscopy and fungal cultures. This will allow the doctor to determine whether it is a fungus or another condition, such as lichen planus, psoriasis, nail damage, and onychogryphosis.
Fungus in the nails can be hard to get rid of with over-the-counter drugs. This is due to the nail being hard and protective, with fungus able to slip between the nail bed and plate. Furthermore the slow growth of the nail increases the difficulty of fungus going away. Laser treatment seeks to get around this by directly penetrating through the nail and killing the fungus. The laser is used on each infected nail for a couple of minutes. Patients then typically return several weeks or months later for another laser treatment. During this time the podiatrist will routinely observe the foot and infection. It is also recommended to wear clean socks and shoes and allow the feet to dry and breathe to prevent toenail fungus.
Laser treatment is still a relatively new treatment and not all podiatrists have laser machines. Ask your podiatrist if they do laser treatment for toenail fungus and if it is right for you.
Possible Reasons for Burning and Burning in the Achilles Tendon

Pain and burning in the Achilles tendon are often signs of Achilles tendinitis, an inflammation of the tendon that connects the calf muscles to the heel bone. This condition commonly results from overuse, particularly in athletes who engage in repetitive activities like running, jumping, or sudden direction changes. Wearing poor footwear, improper stretching, or tight calf muscles can also contribute to the development of Achilles tendinitis. As the tendon becomes irritated, individuals may experience pain that worsens with activity or after long periods of rest. In some cases, the tendon may feel warm, swollen, or tender to the touch. Over time, without proper treatment, Achilles tendinitis can become chronic, leading to further damage and weakness in the tendon. If you have sustained an Achilles tendon injury, it is suggested that you promptly schedule an appointment with a podiatrist who can effectively treat this condition.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of New England Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Chelmsford and Newburyport, MA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Featured Articles
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- March 2016